Brené Brown: Hi, everyone. I’m Brené Brown and this is Unlocking Us.
[music]
BB: Wooh! This is a important, enlightening, tough, loving conversation about dementia and Alzheimer’s, and I know many of us have been caregivers and are caregivers, and I know a lot of us are also living some anxiety about it happening to us, and so this week, I’m talking to this incredibly wonderful Alzheimer’s disease researcher, clinician, Dr. Jason Karlawish.
BB: He’s the author of The Problem of Alzheimer’s: How Science, Culture, and Politics Turned a Rare Disease into a Crisis and What We Can Do About It. Again, it’s one of those conversations, y’all know me by now, it’s going to get very personal very quickly, and it’s personal for Jason as well, but he’s also this incredible leading expert, and he really just breaks it down for us and teaches us so much, and I do think, in this case, that knowledge is power, especially when it’s knowledge that, not only comes from biological and medical understanding, but this is a heart-centered guy that talks about the reality of this disease and the caregivers.
[music]
BB: Before we jump in, let me tell you a little bit about Jason Karlawish. Dr. Karlawish is a physician and a writer. He researches and writes about issues at the intersections of bioethics, aging, and the neurosciences. He’s the author of the novel, Open Wound: The Tragic Obsession of Dr. William Beaumont, which is actually a fiction book, which I’m going to read soon, I can’t wait.
BB: His essays have appeared in The New York Times, The Washington Post, Forbes, The Philadelphia Inquirer. He is a professor of medicine, medical ethics and health policy, and neurology at the University of Pennsylvania and co-director of the Penn Memory Center where he cares for patients.
BB: He lives in Philadelphia, and you’ll meet, maybe, I don’t know, an hour in, you’ll meet his dog. [chuckle] Which is really fun. I love people and I love when someone like Dr. Karlawish can bring humanity to a topic that feels like it strips the humanity from people and just crushes caregivers. Thanks for being here.
[music]
BB: Thank you for being with us on the podcast today. I really appreciate it, Jason.
Jason Karlawish: It’s a pleasure to be here, Brené.
BB: I will have to say to everyone, I went through this Dr. Karlawish or Jason thing and of course, he said, “Whatever you’re comfortable with.” And I want to share with y’all why I’m choosing Jason. I’m choosing it because there’s this brilliant book that we’re going to talk about that Jason has written called The Problem of Alzheimer’s, and I feel like everyone in the world needs to read this book, whether you’ve been personally affected yet or not. But it also feels super personal to me, and I’m trying to maybe minimize some distance so I don’t just get data-nerdy because I’ve got a lot of data questions and nerdy questions, but I’ve also got a lot of hard, personal questions. So this is my attempt to do that with you, if that’s okay.
JK: Yeah no, Jason becomes like the mediating word to kind of balance between the science and the personal, yeah.
BB: Yeah. I want to start with this question, and we start here always. I would love you spend the first 10 minutes just tell me your story. Where are you from? How’d you end up here?
JK: Yeah. I grew up on the East Coast in the Tri-State Area, which meant we lived in the commuters’ town to New York. My father took the train in to work on Wall Street, and then probably, one big event in my life was I went West. [chuckle] I went to Northwestern to study and got out of the East Coast, and that was I didn’t even, I didn’t realize, so much of the time, how much that made a difference for me to broaden my perspective on America and the world. Studied in Northwestern, and the key thing there was I was in a program that…
JK: I was already in med school, and so I spent three undergraduate years, yes, doing the pre-med requirements, but with none of the psychological baggage that surrounds pre-med, and I could really explore my interests in humanities, history of science, philosophy, ethics.
JK: And those three years were critical for the remaining years. [chuckle] It’s why we’re here today, in some sense, because I really created a grounding of understanding in the humanities, knowing I was going to go to med school. Went to med school in Chicago at Northwestern, and then anyway, ultimately, would train in internal medicine and geriatric medicine, and now, I’m on faculty since I finished my fellowship in 1997 at the University of Pennsylvania.
JK: Another key event in my life was I was actually going to become an intensive care doctor, and when I was at the University of Chicago doing my bioethics fellowship, I was matched also in a critical care fellowship, but I dropped out and switched to geriatric medicine, and I chronicled that in the book, and it was one of the pivotal events in my life, surrounding personal events, my grandfather had Alzheimer’s, but also, some professional and larger intellectual events, as well that have me say, “We definitely need more intensivists.” Boy, have we seen that this past year. [chuckle]
BB: Yeah.
JK: But we really need people to help take care of America’s aging population, especially those who are disabled by dementia, and that was kind of my calling moment, when he was basically killed by an academic medical center. So anyway, been on faculty at Penn. I co-direct the Penn Memory Center. I see patients every Friday for diagnosis, treatment, and long-term follow-up care, and the rest of the week, I run a lab called the Penn Program for Precision Medicine for the Brain, and we study issues at the intersection of ethics, policy, and science. We’re really interested in biomarker transformation of Alzheimer’s, and I’m sure we’ll talk more about that, and I’m a writer, I write essays, I wrote a novel, and then of course, this book.
BB: So this explains so much to me, to be honest with you, and I’ll tell you what it explains to me. As someone who, I took care of my grandmother, and her care was really awful, and we didn’t know what we were doing. It was painful and traumatic, and I’m sure like many people listening, she’s not the only person in our family with dementia. I connected with your work. I want to understand this disease from someone who is a physician, who understands ethics, who speaks policy, and has a heart full of liberal arts and humanity. Do you know what I mean?
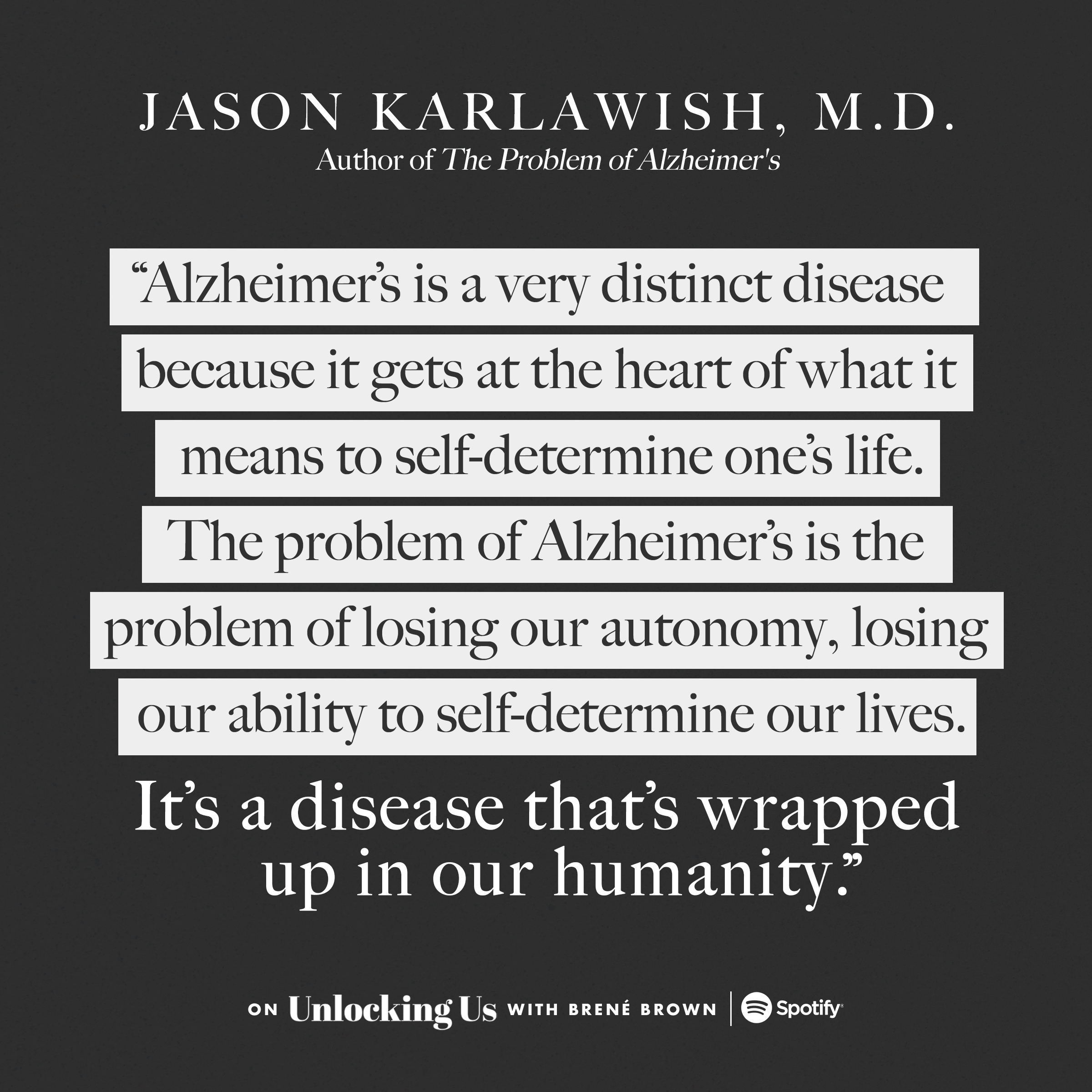
JK: Well I was trained never to accept compliments, so I’m not obliged to say I know what you mean. [chuckle] But it is a disease that’s a humanitarian problem, that’s one of the points I make in the book, and it’s a very distinct disease because it gets at the heart of what it means to self-determine one’s life. In other words, that’s why it’s a disease: There’s this pathology going on, and that explains it biologically, but what the problem of Alzheimer’s is the problem of losing our autonomy, losing our ability early on to self-determine our lives.
JK: And so it’s a disease that’s wrapped up in our humanity and therefore, the humanities are essential to understand, make sense of, live with this disease. So yeah, I know. I get what you’re saying, I do, and the stories I have in the book aren’t just stories to embellish and add a little color in between the… They’re essential to make sense of the disease, the stories of patients and their families. Yeah, I agree.
BB: I’m going to start with this, and then I want to jump into the book and I want to really spend some time in the beginning with the Harrisons, and I want to spend some time with the Harrisons because I have a lot of questions. In the end, what I want you to tell me is that every doctor’s office will have like a scanning machine, will be able to reliably and accurately predict where you are, there’ll be a great drug to stop it in its track, and some supplements and diet to reverse it. That’s where I want to end this conversation.
JK: Okay. [chuckle] I think one of the central points I arrived at in my career, and frankly, many of my colleagues’ is this is a vast and all-encompassing problem, a very heterogeneous problem, the problem of Alzheimer’s, and we’re not going to drug our way out of this. This is not like COVID where there’s not but one, but three effective vaccines in less than a year, okay? This is not like polio. This is like cancer, this is like heart disease. We should expect progress in therapeutics and diagnostics, spectacular progress, I think, and I can talk about that. But we’re not going to look back on this disease the way we look back on polio.
BB: We’re not, right?
JK: No. See, “We’re not cynical, you don’t believe in science, you’re… ” No. If you look at the heterogeneity of what causes dementia…
BB: I’m going to stop you there. What do you mean by the heterogeneity of what causes dementia?
JK: Yeah, you’re good. You caught me. [chuckle] Well, dementia means disabling cognitive impairments, okay? So multiple parts of cognition are impaired; memory, executive function, language, and they’re impaired to the degree that you can’t do your usual and everyday activities; make a meal, plan a trip, organize your medications. That’s dementia. Many different diseases cause dementia; the most common is Alzheimer’s disease, but there are other diseases.
BB: I’ve got to stop you right here. I want to make sure I understand what you’re saying because this book freaked me out in how much I had misunderstood. Many diseases cause dementia; Alzheimer’s is one.
JK: That’s right.
BB: I thought you had to have dementia to have Alzheimer’s.
JK: Once upon a time, that was the case. Once upon a time, my field, medicine, said, “First, you say someone has dementia, and then you figure out the cause of it.” And the most common cause was Alzheimer’s, that’s true, and that is changing, we’ll talk about that.
BB: Okay.
JK: But I think the key point I’m getting at is what the Harrisons raised to me, which is a couple who opened the book, is the most common question you hear when you give a talk in the community, when you meet patients and family members at the Penn Memory Center, etcetera, is: What’s the difference between Alzheimer’s disease and dementia? And the difference is dementia describes disabling cognitive impairments. Alzheimer’s disease is the most common cause of those disabling cognitive impairments. It’s the most common disease that causes dementia. But there are other diseases that cause dementia.
JK: Lewy body disease that Robin Williams had, he had Lewy body disease, distinct disease. Frontotemporal lobar degeneration is another cause. Parkinson’s disease causes dementia, particularly in individuals who develop it after their sixth, seventh, decade of life. Huntington’s disease. HIV infection, if left untreated, causes dementia. Syphilis, if left untreated, can cause dementia. So there’s a whole different set of diseases.
JK: Now, with a respect to Alzheimer’s, one of the stories I tell in the book is, even the disease we call Alzheimer’s disease, we have discovered, is more complicated than just two simple pathologies at work, but rather, there’s a variety of different pathologies at work, depending on one’s age and other illnesses that they have, and again, we’re getting in the weeds quickly, but the point that led us into these weeds already is the idea that we’re going to cure the problem of Alzheimer’s, the problem of dementia, is I just don’t think a rational policy for society.
JK: We should pursue better treatments, definitely, in therapeutics, but to say, “We will cure it,” I think sets us up for false hopes, and it’s a little like buying lottery tickets to plan your retirement. You may win. If you do, you’re going to win big, but the odds are you’re not, and then you’ve wasted all this energy and money on a goal that you just weren’t going to get at. So I am not anti-treatment. We have to make more progress in therapeutics. But I don’t think it’s fair for me and you to have a conversation with your listeners, believing, “Oh, we’re just going to cure this, we just need a little bit more time.”
BB: Right.
JK: It’s just not fair. Just like we haven’t cured cancer and yet, we’ve made spectacular progress on cancer. But it still remains a vexing disease, so, too, cardiovascular disease.
BB: That’s so helpful, and especially married to a non-interventionist pediatrician, I am not a “let’s label it and drug it as fast as we can to get rid of it” kind of person, but it feels like… And I’ll be honest with you Jason, I’m 55. At least 50% of my friends are caregivers for a parent who has, I guess, some disease where dementia is showing up, and so is there this fear that gets in the way of doing what we can do because we want a miracle cure?
JK: Well, I think there is a fear of the disease, a stigma that surrounds the disease, even, that makes it difficult for America to rationally and, I think, humanely take on the disease. I mean this disease is haunted by stigmas, the stigmas of either developing the disease or becoming a caregiver for someone with the disease, and let’s talk a bit about the caregiver because I think of all the diseases out there, this is a disease which, early on, creates, and my rhetoric is strong here, creates another patient, that is to say a caregiver.
BB: Yes.
JK: And I say “another patient” because many caregivers will talk about not just the work of care, and it’s a lot of work, but also, the emotional burdens of care; some of them even developing depression and anxiety, sleep disorders, their own other health problems, as well, forgoing their own care in order to give care. I would be loath to sort of medicalize the role of caregiving, but I do think we need to acknowledge that caregiving, particularly for someone with dementia, is morally, physically, spiritually-challenging, and one of the points I bring out in the book is we don’t support caregivers like we need to as a society.
BB: No.
JK: We have done a poor job in that, and it’s a chronicle of 40 years of misadventures, and most of it politics, frankly, in our effort to… Failed efforts there, yeah.
BB: Yeah, definitely. I went through every human emotion reading this book, and we’re going to talk about the politics and the policy issues, especially of the 80s.
JK: Yeah.
BB: That’s where I flagged as my rage section.
JK: Yes, yes, anger. I had an interviewer say, “You seem angry.” I’m like, “Yeah, I am angry. I am. We missed so many opportunities.”
BB: Yeah, no, we’re going to get there.
JK: Yeah.
BB: Let’s meet the Harrisons because I feel like, and this is where you can really see the power of narrative prose that you have from those great days at Northwestern, because this is a tough story. So you meet the Harrisons, and I make up, and tell me if I’m wrong, I make up that you share this story because a lot of us see ourselves in it, and it’s a very common narrative about… Is that true?
JK: Their story is very typical, very typical.
BB: Okay. One of the things that happens is, it’s really interesting, you interview the family, you talk to the family about what’s happening because your experience and my experience, too, is the person experiencing this will downplay it, minimize it.
JK: Yep.
BB: But family members are somewhere between concerned and freaking out, right?
JK: Yep. The most important technologies in a memory center are chairs because you need to have room to accommodate not just the patient, but someone else who knows the person well, and that’s right, it’s routine in a memory center. This isn’t just the one I practice at, but memory center’s writ large, and I chronicle other ones in the US, elsewhere, is to have someone else come in with the patient to provide, in my professional language, you call it collateral history. There are a knowledgeable informant, quirky terms, to be sure, but they describe that role of the spouse, adult child, daughter-in-law, typically, to tell what they’ve noticed.
JK: And the reason is, and it’s grounded in the recognition that individuals with cognitive impairment, number one, often have apathy and so, lack the initiative to get help and/or have trouble getting help, namely, “Let’s make the phone call and make the appointment.” And number two, have trouble narrating the full panoply of the problems they’re experiencing it. Typically, they’re aware there’s a memory problem, but they have… It’s fascinating, difficulty seeing the significance of it in their life, recognizing the disabilities. So that’s why we seek out an informant, and frankly, the other reason why we seek out an informant is if we do diagnose cognitive impairment, we need that person to transform into a caregiver, which is what, of course, happens to Mr. Harrison for his wife; he becomes her caregiver, as does his daughter.
BB: So what happens here first is some of the signs that people are talking about, this informant are talking about with you, in my own experience, for sure, too, bank balances look weird.
JK: Yep, money, meds, telephone, technology, transportation. [chuckle]
BB: Wait, say that again.
JK: Yeah, it’s what I do with teaching to residents’ families in the community. You want to figure out whether someone’s having potentially worrisome cognitive problems that need evaluation: Money, medications, technology, transportation. Are they having trouble managing their money, their medications, using technology like the computer or the telephone, etcetera, assuming they used it before, and transportation, namely, getting from point A to point B. And most folks who sort of reflect on that with someone they know who has dementia, whether it’s caused by Alzheimer’s disease or other diseases, will say, “Yeah, yeah, the first signs were the checkbook was no longer balanced.”
JK: Or, “No more long trips, just short trips.” Or, “Constant back and forth to the pharmacy to clarify the prescription.” Or, “He kind of got confused with the iPad when it used to be okay.” And it makes sense because the earliest problems caused by cognitive impairment are troubles with what we call executive function and multitasking and memory, working memory, and those are cognitively demanding activities. The key point, I think, is oftentimes, when people hear Alzheimer’s disease, especially Alzheimer’s, they think someone who can’t bathe, dress, groom, feed, and toilet.
BB: Say that again, and slowly?
JK: Yeah, no, that’s the doctor… [chuckle]
BB: No, it’s super helpful, but I’m trying to listen to you and breathe at the same time, which is hard because it’s so resonant. So when we think Alzheimer’s, we think?
JK: Many people jump to what I would call the severe stage of the disease, someone who needs help with bathing, dressing, grooming, feeding, and toileting, and that’s what they think of when they hear the word “Alzheimer’s.”
BB: Yeah.
JK: And it is the case that if someone has the disease and lives long enough with it, many patients do need help with bathing and dressing and grooming and feeding. Many do, not all, if they live long enough. But that describes the last third of the disease. The first two-thirds are trouble self-determining your life in the community. They are trouble ordering off of a menu at the restaurant. They are trouble deciding which medication to take when given options for medications. They are trouble organizing care, if you’ve got to go see a bunch of doctors. They are trouble making financial decisions, which is where the scammers or the fraudsters are, unfortunately, targeting our seniors.
BB: Special place in hell for those folks.
JK: Absolutely. I’ve got a family member recently who was defrauded, for example. But anyway, those are the early stages, and that’s why this disease is so dreaded. I mean of course, there’s extreme disabilities of severe-stage disease, but it’s this loss of self-determination which makes the disease so uniquely dreadful, which early on, it chips away the cherished value in our lives, which is we choose to live the way we choose to live. Each of us are sitting in our rooms decorated the way we chose to decorate it with the things we want and that we bought and that we picked out with or with other people as well, and this disease, early on, chips away at those very cherished values of exercising your autonomy, early on.
BB: When I read that, I have it highlighted where you say this, it’s on top of page 11: “Dementia, in a sense, is a disease of autonomy, and the lives of persons with it are in extended conversation over a question: What’s a good life when you’re losing your ability to determine that life for yourself?” Oh!
JK: Yeah, you found one of the pearls in the book, you’re right. That sums up: What’s the problem of dementia? Exactly.
BB: Jeez! So I want to get to this other highlighted place where I had such a personal reaction to this. Mrs. Harrison, I think they get a call from the homeowners’ association, if I remember right.
JK: Didn’t pay a bill.
BB: Yeah, they didn’t pay a bill. Those kind of things are happening, and then, can I read something to you from your book?
JK: Please.
BB: “Mr. Harrison pushed back when I labeled his wife as mild stage. ‘Her anger, it’s so disruptive. This has to be severe’, he countered. ‘The account or severity of the emotional and behavioral problem is not factored in to staging,’ I explained. ‘The focus is function and cognition because they best predict what to expect in the future, and the time that will pass between diagnosis and death.'” Can you unpack this for us?
JK: Absolutely. Staging means how sick is someone, where are they at, and what’s going to happen next, and when we stage dementia caused by Alzheimer’s disease, for example, we look to function, we look to someone’s ability to perform their usual and everyday activities: Managing their money, managing medications, transportation, technology, how impaired are they doing those things, and the degree of that impairment describes going from mild to moderate-stage dementia. Severe stages, troubles now with picking out clothing, putting it on, washing up, using a knife and fork, etcetera. Behavior problems are very common in persons living with dementia. By the way, I know someone who’s living with dementia may object to me saying, “Behavior problems,” but sorry, I realize that’s… I’m sensitive to that.
JK: But anyway, apathy, lack of initiative, anxiety, depression, anger, false beliefs, delusions, those occur. But they wax and wane like the moon, that is to say they don’t get worse and worse and worse. In the moderate stage, the patients may develop a lot of agitation, but then, that sort of waxes away. I have patients who, early on, have a lot of anxiety and that, oftentimes, waxes and wanes as well. So we don’t count the severity of those kinds of problems to stage how ill the person is, and what to expect in the future, etcetera. So that’s doctor talk.
JK: But what Mr. Harrison was saying was, I think, something that’s very real and I think you have to acknowledge it. Things like anger, apathy, etcetera, from the perspective of someone living with the disease or living with someone with the disease, that describes, oftentimes, how bad it is, not to discount the functional deficits, but it’s the anger and the apathy, which oftentimes, makes it, sort of, if you will, difficult for others.
BB: This paragraph that I just read that we’ve just unpacked, to me, really makes the case for two patients.
JK: Yeah.
BB: So I think you will look at me and say, “Hey, Brené, I think your grandmother’s at a mild stage. I think you may be at moderate caregiving fatigue.” [chuckle]
JK: Yeah.
BB: They don’t always match, right?
JK: Yeah. I quote Arthur Kleinman in the book, a psychiatrist, an anthropologist who was caregiver for his wife, and he writes how, “She’s happy, most of the time; it’s me who’s suffering.” And that statement resonates, I think, with many caregivers.
BB: Oh, God, yeah.
JK: Yeah.
BB: In the home where my grandmother ended up, there were some very common things you’d see in rooms, and I want to ask you about this because this is just a personal question that I get to ask you because I get to meet you. You would see signs in people’s rooms that said, “We’re all still here, this is where you live, and you don’t owe anyone any money.”
JK: Yeah, yeah. [chuckle]
BB: Is that common, the worry?
JK: Yes, I chuckled at the “You don’t know anyone money.” It’s interesting how many caregivers will tell me about how their relative worries, you know, “Have we paid for this? Are we up-to-date on the bills?” etcetera, and the need for the reassurance around that. It’s so tragic to hear that. Think about what that says. It says that the person living with dementia, as disabled as she or he is, still has sort of a sense of responsibility, a sense of sort of duty, a sense of worry that they haven’t done the thing that they’ve always done all their life, which is “pay my bills,” and as annoying as that repetitious question may be for the family member, it’s one of those questions that I think reveals the humanity, the identity, the personhood in the person living with dementia, they’re still worried about that bill, “Did we pay those bills? Are we okay?”
BB: It’s a beautiful frame on it, really, Jason, that these folks that are in this struggle are still feeling a sense of responsibility about the things that maybe they prided themselves on being good at.
JK: Yeah, and I say that, by the way, not to make the disease any better than it is because all disease is bad. I keep on saying “persons living with dementia.” Do you notice that?
BB: Yes, yes.
JK: If you had interviewed me five years ago, first of all, I could never have written this book. Well, “never” is a strong word, but I would have talked about people who are demented.
BB: Really?
JK: I would have been adjectival. Oh, yeah. Oh, we used to say that routinely, “Oh yeah, you know, he’s demented, yeah. You know, well, among the demented.” And a change that occurred in my, and many of my professional colleagues I’ve noticed this has happened, we’re very now effortless in saying “persons living with dementia,” and I’ve noticed this is occurring in the field, and it’s a very important, I think, linguistic turn.
BB: Yes.
JK: Which is to go from saying, “Oh, he’s demented.”
BB: Right.
JK: To saying oh he’s a person living with dementia because that very word, that very phrase is an effort to do just that, bring out the personhood. Of course, recognizing that their personhood is being threatened. But one way that we can, if you will, counteract that threat is to acknowledge that they’re still a person, albeit perhaps, in care.
BB: As a social worker that would be in grand rounds, I would be very appreciative. [chuckle] I would be like, “Yes, with!” This is an interesting place to ask you this question. Tell me about how the progression of working titles for this book reflected your own journey. Is that a fair question? Is that okay?
JK: That’s interesting. How did you know that? Because it’s true, I had this interesting progression of working… I have so respect the idea now of working titles. It’s thousands of words and yet, in the end, a title makes you move it along. It’s fascinating when you think about it. So the original title for this was My Profession: Confessions of an Alzheimer’s Doctor, or My Confession: Professions of an Alzheimer’s Doctor, which is classic Karlawish wordplay on the idea of profess and confess.
BB: Yeah.
JK: But anyway, it was a sort of effort to try and say, “I am an Alzheimer’s doctor, and I’m in this profession and yet, things haven’t gone that well. Why are we in a crisis?” So that worked for a while, but what I didn’t like about it was that, it risked being too much about me, and I didn’t want to write a book about me, and then it became The House of Alzheimer’s Disease, and I liked that title for a while. In fact, that’s the title I sold the book with, my agent and I, because it is a disease that, in some sense, is constructed.
JK: It’s a real disease, and I push back against the social construction, as you say, “This is all just a social construction, and if it could just… ” No, no, no, there’s a reality to this disease grounded in biology. But what we call the disease, how we respond to it is something that is by our own acts as humans, and that’s the crisis, if you will. That’s why it was called The House of Alzheimer’s; we built it, we made it the way it is. I also like “the house” cause it evokes idea house in terms of nurturing, and home, and creating a space, that we can make a space for people with Alzheimer’s.
BB: Yeah. It’s a powerful title.
JK: And so that worked for a while, and I remember my agent, David McCormick, saying, “Eh, you know, you’re going to change that title.” And he’s right, we did, and then we changed it to The Disease of The Century, based on an essay that opens the book by Lewis Thomas, a very famous physician and college history researcher and author in America in the late 20th century, and that title worked for a while. In fact, I was sitting at a socially-distanced gathering and I said this to someone “Yeah, I got my book coming up, The Disease of The Century“. Like, “Oh, it’s about COVID?” I’m like “No, it’s not about COVID.”
JK: So then, I said, “Oh, my God! I’ve got to get a good title,” but I like this title because The Problem of Alzheimer’s is the problem. It is that is the issue. We have this thing called The Problem of Alzheimer’s, not the problem of dementia, and then the subtitle really tied it up, which is How Science and Culture Made it a Common Disease, and then Politics Turned it into a Crisis. So that’s the title, How Science and Culture and Politics Turned A Rare Disease into a Crisis and What We Can Do About It. So yeah, it’s interesting. As a writer, the work… I really walked away with “working titles are really important,” and be ready to surrender them.
BB: They’re so important.
JK: But be ready to get rid of them, that’s the key. I think as a writer, you could relate. You’ve got to know when a specific title’s so not working, you know? [chuckle]
BB: Totally. It’s painful. But I ask writers often, I don’t usually ask super medical non-fiction writers, but I don’t consider you in that list. I think you’re a writer’s writer. I think you’re a writer, and you happen to be a doctor. That’s how I would see you because I’m a writer. But the progression, normally, it’s therapeutic, in a way. It’s about the growth and where you are in relationship to the content, I think.
JK: To use another word, the turning that occurs as a writer when you’re creating a work. I like the word “turning,” as opposed to “revolution,” although revolution is turning, revolves, and it requires a lot of self-inquiry to know, “I’ve arrived at a different place in terms of what I’m writing about, but it’s because I’m creating it, which is great, and it’s moved in this new way, and that’s a good thing, so let’s change the title.”
[music]
BB: Okay, here’s what I want to know about. I want to know this story. It’s going to be a tough story, you’re going to have to translate it for me because it’s pretty technical, but there’s something important for me in this story. I want to understand the cluster that was the Eli Lilly meeting. I want to understand that. Can you explain it to me as a lay person?
JK: Oh, my gosh! Yeah, the January disaster, yeah.
BB: Because this is part of my wish list, is I want a scanner that becomes a standard of care in every internal medicine doctor’s room. But is that what’s even in play here? Is Eli Lilly saying, “Hey, we’ve got a scanner that you can use.”
JK: So the first part of the book, I tell the story of the transformation of Alzheimer’s disease, from a diagnosis based on people like me doing careful, meticulous histories and exams, to a diagnosis based on doing tests that pick up the biomarkers of the disease, and I tell the story of the first biomarker that kind of broke through, which was the ability to image amyloid, which is one of the pathologies of the brain, amyloid plaques, or one of the two pathologies that are seen in Alzheimer disease.
JK: Using a PET scanner, and a PET scanner is essentially a CAT scanner, but you get injected with a radiotracer, and the radiotracer is picked up by the CAT scanner, and I chronicle these two just fascinating collaborative scientists, Bill Klunk and Chet Mathis, who developed the first radiotracer that picks up amyloid in the brain.
BB: Can I stop you right here and ask you a question? Amyloid in the brain, is that what lay people hear about like, “She’s got white plaque in her brain”?
JK: Yeah, yeah, yeah, the plaques. Yep, those are the plaques.
BB: Okay, got it, okay.
JK: So Chet and Bill discovered this compound, which would become known as Pittsburgh compound B, otherwise known as PiB, and this is a tremendous revolution that occurred at the turn of the century. Anyway, another very young, super smart, highly ambitious guy named Dan Skovronsky would discover another radiotracer that was better for commercial sale, and I get into in the book why PiB can’t really be sold commercially, it’s too hard to manufacture, etcetera. Anyway, in the end, Eli Lilly buys Dan’s company, and that’s a neat story in its own right, and Eli Lilly develops this radiotracer called Amyvid that can pick up amyloids. So this is all very encouraging story, and they have to move it along down the regulatory pathway. They go through FDA and… What they did to get it through FDA, the science they did was utterly brilliant and also revolutionary. It really is a great story. But there’s one more stop along the way, which is they’ve got to get Medicare to agree that, “We’re going to pay for this test.” And this led to the meeting outside of Bethesda of the Medicare Coverage and Advisory Committee, known as MEDCAC, to review the evidence to support whether this amyloid imaging tracer should be paid for by Medicare. “Is there value in this test?” is the question on the table.
BB: Okay.
JK: And so Lilly brings their experts, and others come forward to make the argument that there’s value in this test, and this MEDCAC, which is a very distinguished group of people who do work in health economics, health service delivery, quality of care, very legitimate group of people, and it’s like one of those moments in history where the two different cultures came together and needed to arrive at an agreement, and each presented and reflected upon their…, and they could not agree, and it ends with a decision that the evidence does not support that this test has sufficient value to be used in clinical practice, and again, if you approach that question as someone like me, an Alzheimer’s expert who really knows how to properly identify someone who needs the test and how to interpret it, we could do it with value. The problem is I’m a rare bird.
JK: There are very few physicians like me, and a test like that at that time, widely available, everyone anticipated, and I think legitimately so, it was just going to be widely used and abused and not used correctly, and I think the result was Medicare said the evidence doesn’t support the value for this test, and that still stands today as their decision. What would change that is some evidence that it really is valuable in the hands of the average prescribing doctor, and that would probably have to be a therapy, shown to be effective, that would treat the underlying pathology, which we don’t have.
BB: It brings up the point of it’s not about a valid and reliable output from a testing machine, in my mind.
JK: Oh, yeah, they totally agreed it measures amyloid, no one doubted that.
BB: It’s about, “Is the training sophisticated for the general practitioner to be using this in a way that’s helpful to the public?” Is that their question?
JK: That’s exactly what the problem was. That’s exactly what the problem was, and if you took doctors like Dr. Solway or myself, Solway was one of the doctors that testified at the hearing, and he got angry. But it was like, “Well, yeah, no, Solway.” “Well, yes, Steve, you can use this well.” “But if this test is widely available, it’s not going to be used well.” And the reason why is because America never invested and still does not have an adequate physician workforce to diagnose and care for people with dementia.
BB: Oh, God! That’s true.
JK: To diagnose and care for people with Alzheimers, and that is the problem, that is why we have a crisis, and if you think about it, as I write in the book, if we lived in a world right now where all these older adults were showing up anemic, fatigued, etcetera, and doctors are like, “Oh, my God! You’ve had undiagnosed… ” and it is going on for two years, bouncing from doctor to doctor with no clear answer until finally, an oncologist says, “Oh, my God, you have undiagnosed cancer for two years. You’ve been seeing how many doctors and they didn’t diagnose?” We would see this as a scandal.
JK: But that’s what’s going on in America now, that the typical American wanders around for one to two years, bouncing from doctor to doctor, getting incomplete answers, half truths, or just “I don’t knows,” until finally, they landed a physician who knows how to work up cognitive complaints, and that’s not to indict American medicine, to indict a healthcare system that never invested in training physicians to do that kind of work. This is where you get angry. [chuckle]
BB: Yeah, I’m moving into rage stage.
JK: Exactly. [chuckle]
BB: He can see me because we’re on Zoom, so we can see each other, and my arms are up and in the classic anger pose.
JK: Yeah, yeah, “We’ve got issues!”
[chuckle]
BB: I’m in classic rage pose. So you write, let me see if this makes sense, and you may have to offer some context, but it just jumped out at me. So diagnosis, stage, education about the diagnosis and stage, this is the goal, right? And this goes to not enough people trained to diagnose, stage, and then educate. This is what you write. Then support to develop a day that’s safe, that’s social, and that’s engaged. This is the part that pissed me off. You don’t leave the diabetologist’s office, I guess that’s a doctor who deals with diabetes. Yes, I’m going to say this: You don’t leave the diabetes doctor’s office with a prescription for an anti-diabetic drug and then say to them, you know, “Good luck. Hope you figure it out on your own.” When my husband has diagnosed people with diabetes, these folks, not just the young patients, but their families, their grandparents, they’re going to classes, Steve’s meeting with everybody before the class and after the class, and then there’s check-ins, but that is not my experience in my family.
JK: With dementia.
BB: Yeah, with dementia, and so when you say that we’re not trained, I want to say this to you, and I want you to tell me this is accurate or not accurate. We need more medical professionals, probably not just physicians, but across the medical board, trained, deeply trained, humanity, ethics, and medicine trained to be able to diagnose, to be able to stage, to be able to educate the diagnosis and stage, and then we need a complete support system in place that helps caregivers provide safe, social, and engaged care.
JK: That is the standard of care, that should be the standard of care, and that is not the delivered standard of care in America right now, and that’s a problem. Why? It’s a many hydra-headed story, but there are a couple of key reasons. I think one of them, back to the diabetes analogy, is Alzheimer’s disease has never enjoyed a good business model, and in America, a disease isn’t fully a disease until it has a business model to sustain it and support it.
BB: This pisses me off.
JK: Well, that’s what we set up. We could change it. This is all politics. [laughter]
BB: So there’s not a good money model.
JK: Yeah, if a disease doesn’t have a good business model, it’s not going to be widely picked up and treated and identified by the American medical system, and Alzheimer’s certainly is one good example of that. Quite simply, the amount of time and effort it takes to do the evaluation care you need is just not adequately reimbursed, and so the typical physician can’t spend the amount of time that’s needed to do work up, and we just don’t have a system of long-term care services and supports to provide the education and support to a family to create a day that’s safe, social, and engaged. All of these are fixable things, we just have to invest in them.
BB: If you’re listening, if you’re on your walk right now or you’re driving to work, let’s take a collective deep breath before Jason tells us about the ’80s. Let’s just take a deep breath and so walk me into the series of policy nightmares that led to where we are now.
JK: 1980 comes around. In 1980, seven dedicated families get together and formed the organization that would come to be known as the Alzheimer’s Association. These were families, granted they were very closely aligned with physicians, but these were family members that said, “The system is not treating my family well, I can’t get a diagnosis, I can’t get care.” Their stories are harrowing, harrowing stories. They formed the Alzheimer’s Association, they’re determined to raise awareness, make people aware that senility is not extreme old age, but actually is caused by a disease and that’s Alzheimer’s disease, get Congress and NIH to focus on this disease research and get Congress to support care, namely long-term care services and support systems.
BB: Long-term care services and supports, what does that mean?
JK: That means just like Medicare pays for your healthcare, your medical care, that Medicare would pay for the training that a family needs to put together a day that’s safe, social, and engaged, help support access to adult day activity program, help support a family member to provide daily long-term chronic care to their relative. Long-term care social insurance that exists in most developed nations, Germany, etcetera…
BB: Yeah, this makes complete sense, yes.
JK: Yeah, Japan has a program…
BB: Who can be against it? Yeah.
JK: Well, that’s where the ’80s come. So at the same time that it occurs in 1980, Ronald Reagan is elected President. Reagan and his administration would not pursue policies that were explicitly “Anti-Alzheimer’s,” that are designed to make the lives of caregivers like Hilda Pridgeon, who was one of the founders of the Alzheimer’s Association, miserable. But their policies had that side effect because what would happen in the Reagan years and then decades that would follow, would be this tense conversation around, “We need to shrink the size of the federal government, deregulate it, devolve things back to the States.” Medicare and Medicaid were viewed as wasteful bloated programs that needed to be cut, and there was zero appetite for expanding social insurance programs.
JK: And so whatever unity that existed going into the ’80s around the need for a long-term care social insurance program would essentially evaporate by around 1988, and 1988 emerges as a key year in the story of Alzheimer’s, because in 1988, there was an open election in America, Reagan’s term limited out, and every Democratic and Republican candidate was interviewed by an advocacy organization called Long Term Care ’88, who was dedicated to getting this long-term care social insurance passed in America, and every Democratic and Republican candidate had to line up behind that agenda…
BB: That’s great.
JK: Except for one, and his name is George Herbert Walker Bush and he would, of course, go on to win the election. What would follow would be the years of “Read my lips: No new taxes,” which would culminate in its sort of policy fulfillment in the Gingrich Congress, which was vehemently opposed to any expansion of the federal government and the expansion of the taxes in order to pay for long-term care social insurance program like through a payroll tax, which is how you have to do it.
BB: Right.
JK: So basically, the 20th century was essentially a political stalemate that Congress cannot agree on how to provide long-term care services that supports the American family, and then the final bit about the ’80s to make you angry is, continued frustration with increasing the research budget to adequately fund the research that’s needed to finally expand the researchers base, the number of physicians and scientists doing research in the space, as well as supporting their research, and that would not occur until about 2010 with the passage of the National Alzheimer’s Project Act, signed into law by President Obama. So the ’80s from 1980 and beyond, when the disease is recognized, was the same time that in America, we entered a political conversation that just became a pitched battle for progress in the Alzheimer’s movement.
BB: What’s frustrating to me about this, Jason, this is my channeling my rage into very proper-ness here, is it’s not like the only caregivers I know are tax-and-spend Democrats. My friends that I know that are struggling, you have to have a shit ton of money to self-finance a parent.
JK: If you’re extremely rich, you’re okay, or if you’re poor, Medicaid will step in, but the services there are on a waitlist, but for the vast middle class, the neither rich nor poor, they’re left on their own for a disease that can cost up to $180,000 a year. The crisis of Alzheimer’s is a crisis in our economy. It’s a crisis of unpaid caregiving. The triple digit billion dollar figures when people say, “Alzheimer’s is costing America 250 billion a year.” Okay, what lets you get to that number is you take the time that you spent caring for your mother and you turn that into a wage that you could have otherwise earned if you were doing podcasts, educating hundreds of thousands of people.
BB: Yeah, yeah.
JK: And that wage added up across all those many caregivers of the, “I could have been working, but instead I was doing care or I was paying someone else to do the care, okay, so I kept on working, but I… ” So that’s how you arrive at the triple digit billion dollar cost of this disease, and so the complaints that you hear of, “Well, we can’t afford a long-term care social insurance program,” is that we’re already spending that program. The American family is bearing this bill. The American family is suffering alone. Now, I think one of the problems that’s occurred, and I do think this is one of the sort of silver copper linings of COVID is, we’ve realized what it means to be a caregiver, and when a system doesn’t work for you to help care, how bad it could be, suddenly all of us were sort of needing care or giving care this past year, in ways that were sort of like the lives of persons living with dementia.
BB: Yes.
JK: And I think maybe that recognition will allow awakening of Americans right and left to realize that caregiving is a distinct duty. Yes, it’s done by family, because family is best able to give it, but it is a distinct role that needs to be supported with infrastructure, frankly, the way we have roads and other things.
BB: It’s so beautifully put. Just now, thank you, Jason, and so, clearly laid out in the book. Medicaid, but there’s a waitlist.
JK: Yeah, because it’s not a mandate in Medicaid, it’s still a demonstration project which allows Medicaid to say, “We don’t have to give it to everyone who qualifies, because we have just so much resources.”
BB: This doesn’t feel far away from me because I happened to be living in San Antonio when my grandmother was first really experiencing it, and I would get calls at work and that she’s walking down the street… A summer in San Antonio it’s 100 degrees. She’s got on a big coat and cowboy boots, and she’s asking people if they know that her son, my uncle, was killed.
JK: So then you had to leave work, so you were…
BB: No, I did.
JK: Yeah.
BB: I had to leave work until one day, my boss was in tears and said, “I’m going to have to fire you.”
JK: So this is the economic cost of Alzheimer’s. Add that up across 12 million caregivers and that’s why it costs so much, and that’s why when people say, “We can’t afford long-term care social insurance program,” my response is, “But we’re already paying for it.” Brené Brown had to leave her job.
BB: Yeah.
JK: That’s less money she paid into Social Security, that’s less money she has in savings for her family. So we’re paying this bill, it’s just that it’s the American family that’s bearing the bill in a way that’s unfair, uneven, and unjust. We have to have a system that recognizes solidarity. We can’t put the burden simply on the American family.
BB: No, and for me, at the time, I’d go to her house and there would be cigarettes burning that she forgot about, or the stove would be on, and then I was like, “Let me bring her to my apartment.” But I lived on the third floor. Because what happened was like, we’ve got to find a nice place for her.
JK: Yeah.
BB: Well, I mean, her husband was a forklift driver for a brewery. She was a beautician, but they didn’t qualify for Medicaid, they were both retired. So then we’re like, “Oh my God, we have to pay for it.” So that she ends up in a place that’s really all about, to be honest with you, a lot of Benadryl at night, securing your hands to something on the sides, and a lot of Ensure. So what did we say? Safe, social, engaged?
JK: Yeah.
BB: Zero for three.
JK: Yeah.
BB: Like hell…
JK: Yeah.
BB: Hell on earth. But I think, one of the things for caregivers too, is, I mean, you have to agree, there comes a time when you’re loving someone with dementia, that safety prevents them from living with you.
JK: By the way, your story is moving and sadly, all too common.
BB: Yeah.
JK: Add that up and that’s why it becomes as a tragedy, writ large. Having said that, one of the terms I coined in the book or created was “home looseness.” It helps me understand what a dilemma that families face, which is home just isn’t working anymore for the person, and it’s a way, once you recognize this home looseness issue, that they’re not homeless, but just the place that we would think of as home just can’t work anymore. You need to create a new home, and that’s why, frankly, one of the points I make in the book, maybe not as explicitly as perhaps I could have, but I’ll make it here now, is we need nursing homes.
BB: Yes.
JK: We need long-term care residential facilities. I know that some say, “We should close them, our goal should be no more nursing homes, care in the community,” and I get it. We definitely should make every effort for people who are not home loose, home-loose, to be able to live in their homes, but particularly for this disease, given the nature of the cognitive problems patients have, sometimes the best place is… I’m going to use a word that will be provocative, an asylum, in the true sense what of an asylum ought to be: A place that truly is safe, separate from the threats of the world around them, and we ought to think about how nursing homes should be structured and run in a way that provide that asylum, and I think COVID showed us again, we haven’t achieved that with the nursing homes in this country, and so I guess I’m making a statement that may have some of your readers again either screech their cars to a halt or whatever, but the doctor just said we need more nursing homes? Well, we need better nursing homes.
BB: Yeah.
JK: Particularly, for persons with dementia. Oftentimes, it is the best place for them to live. I’m not saying that they’re the best places to live the way they’re run now, but there’s a need for them. Absolutely, and I think your experience gestures to that.
BB: Yeah, and you’re not shy. I mean, you jumped right into gender politics in this book, which I really appreciated, because when we talk about better safe places, we’re talking about, with caregivers paid, and these are often women caregivers, often women of color, where these folks are paid a living wage, where they’re trained adequately. When you say more nursing homes, no one wants to copy and paste what exists, we’re talking…
JK: Absolutely not.
BB: About something that’s possible, so…
JK: Yeah. It’s funny you picked up the gender issues in the book. One of many inspirations to help me think about writing this book was the stories of many women, including my mother, and I remember her telling me how when she… In 1960, ’61, went to the bank to get a credit card, they said, “Well, has your husband given you credit?” and she’s like, “Well, no.” Said, “Well, he has to give you credit and then you can get your credit card.” It’s one of many examples of how, in the lives of America’s women, their ability to claim their autonomy finally, and their self-determination, is what, A, made us, I think, begin to recognize that the disease that takes away autonomy is a disease, it’s not just normal aging or natural aging…
BB: Oh.
JK: But number two, I think, it all the more shows why I think this disease is particularly dreadful for America’s women because they’ve struggled to gain their autonomy, number one, and number two, they oftentimes are in the role of the caregiver, and so therefore, are the frontlines of our lousy system. I had someone else ask me, “So I guess if Alzheimer’s happened to men in their 40s, we’d have a cure now?” I said, “Well, maybe not a cure, but I think we’d have a better system of care.” You know? [laughter]
BB: Yeah, and it’s real, and you do also talk about, I thought this was interesting, that not only if I lose my job, do I lose that income, I lose my health insurance.
JK: Exactly, that’s why the Affordable Care Act is like the Alzheimer’s Care Act, because assuming the Supreme Court didn’t throw it out, it gives the under 65 access to healthcare, which in America, when it was tied to a job, if you don’t have a job because you’re caregiving meant you didn’t have healthcare, which is crazy, but the ACA solves that, as long as we keep the ACA.
BB: Okay, so last question for you before we get to our rapid fire.
JK: Okay.
BB: You say your grandfather had Alzheimer’s.
JK: He did.
BB: Terrible, terrible treatment.
JK: Yeah, he got killed by one of the best academic medical centers after he broke his hip, and they gave him great care, but they gave him lousy care.
BB: I’m sorry. That’s hard…
[dog barking]
JK: Yeah.
BB: That’s okay. We love humanity, including dogs, like my dog’s at home, but…
JK: Yeah, oh my gosh.
BB: That’s okay. Jason has a dog. That’s perfect. For those of us who have it in our families, one of the things that really drives anxiety is this feeling of, “I have a parent or a grandparent who has had dementia, possibly Alzheimer’s, am I next on the list?” Are there things we can be doing now in our lives? What do you do if you have a family history of it? That keeps you awake at night.
JK: All of us, if we live long enough, are at risk of getting Alzheimer’s disease. All of us if we live long enough are at risk of getting dementia. More or less risk, to be sure, depending on things like family history. One of the key lessons that I drew from my research to write the book was, although we don’t have any effective treatments to target some of the diseases that cause dementia like Alzheimer’s, though some day think we will. The last 40 years, we’ve learned very clearly that the risk of developing dementia has been declining. People are at less risk than they used to be, there’s still a lot of people with dementia because it’s so prevalent.
JK: Why has that risk been declining? Well, multiple well-done studies show a variety of lifestyles and other habits that reduce the risk of developing dementia, and actually the AARP has put together what’s called The Global Council on Brain Health, which nicely summarizes what we know now, that does and doesn’t reduce your risk. But simply put, good cardiovascular health is good brain health, and that’s just not about like statins and hypertension, but like smoking cessation, exercise, a Mediterranean diet. There’s good data, unrelentingly good data, that if you can get someone educated to high school, the access and opportunities that follow from that kind of education seem to reduce the risk of developing dementia compared to folks who don’t get beyond a high school education, and multiple studies show this. So yeah, there are things we can do now to maintain our brain health, actionable things, right now, available.
BB: Okay, so I’m going to put you on the spot here. Tell me three or four things you do, Jason.
JK: Oh I like exercise. I’m a big swimmer and runner. I do podcasts with fascinating hosts to keep my brain active, and I enjoy a glass of red wine or two every night. [chuckle]
BB: Okay, alright. Yeah, it’s scary because I have found myself, especially since I’ve hit 50, that if I can’t think of an actor’s name in something, I’m like…
JK: Oh gosh, word finding. Oh, stop!
BB: Yeah, no, I’m like, “We’re here. This is it.” And Steve’s like, “Man, the anticipatory anxiety is going to kill us first.” [chuckle]
JK: Exactly. It’ll only get a little worse when we start having all these biomarkers in practice, but again, that’s part of the… I lay out, we can deal with the threat to our autonomy from learning we’re at risk for this disease, but we do have to take that on as a society, that someday we’ll be able to better predict who’s at risk, and when we can do that, while we’ll certainly have treatments for people to reduce that risk, we have to structure society so that we can live comfortably at risk of this disease and not worry about our employment and stigma, and other threats to our identity.
BB: Yes.
JK: We’ve got a lot of work to do there as a society.
BB: Yeah. Alright, you ready?
JK: Yeah.
BB: Okay, number one, fill in the blank. “Vulnerability is… ”
JK: Needing care and/or getting care.
BB: You, Jason, you’re called to be very brave, but your fear is real, you can feel it right in your throat. What’s the very first thing you do?
JK: I think about how I’ve been fortunate in my life and I think about people in my family who had circumstances that were horrible. My great-great grandfather, who has fought in the civil war because he [chuckle] was paid for by someone who would have been drafted, so he got paid to go fight for the Union, nearly had his life threatened in battle, and then returned and was employed by that man. Anyway, what am I trying to say? When I feel fear and whatnot, I think about how fortunate and lucky I am and what I’ve gotten, my opportunities in my life, the schooling I’ve gotten, the support I’ve gotten, the job I have, the skills I have, and that fear just kind of diminishes, both for what I’ve done, but also how fortunate I am.
BB: Some big time perspective taking, it sounds like.
JK: Yeah, I’m an old soul. [chuckle] I will say that.
BB: Yeah. What’s something that people often get wrong about you?
JK: I think that I’m a writer who happens to be a physician or a physician who happens to be a writer. They’re pretty enmeshed things. They’re pretty enmeshed qualities, the one speaks to the other and they kind of have a dialogue.
BB: Yeah, you can tell that as a reader, for sure. What is the last TV show that you binged and loved?
JK: “Bridgerton”…
[laughter]
JK: And “Great.” I loved “Great.” We loved “Great.” Oh my gosh, I wish there were more seasons of “Great.”
BB: “Great”?
JK: Yeah, it’s the story of Catherine the Great, but it’s got a really hip angle and great costumes and settings, but it’s got a great edge to it. It’s about the story of Catherine the Great. Yeah, but “Bridgerton” and “Great.” Whoever made “Great,” make more episodes.
[laughter]
BB: Okay, you heard it here, right here. Okay, favorite movie?
JK: “The Big Lebowski.”
BB: Oh God, of course. Concert you’ll never forget?
JK: It’s a toss-up between David Bowie or Lou Reed Live at the Tower Theater in Philadelphia.
BB: You saw Lou Reed live?
JK: Oh, it was amazing. Yeah.
BB: Okay, I’m jealous.
JK: He had Antony and the Johnsons on with him, and he sang “Perfect Day.” Yeah, I know, it was memorable, it’s great, it was so cool. I mean, it’s Lou Reed, of course he was cool.
[laughter]
BB: Favorite meal?
JK: Cooked by me, pan fried pork chops in the cast iron skillet and then you deglaze the pan, add a little white vermouth, and from there, you can add all kinds of either savories or sweets, and it makes for a great… Yeah.
BB: Yum. What’s on your nightstand?
JK: I’m reading a very moving book by Kate Washington called Already Toast: Caregiving and Burnout in America, just came out, and Katie Engelhart’s The Inevitable, about the various ways people die in America. Those are a little heavy, but for amusement, I’m also reading this book by János Székely called The Temptation. It’s a story of a young man in Hungary after the First World War, growing up in extreme poverty. You’d think, why would that… Although the particulars are very unique and whatnot, it’s a wonderfully timeless story of growing up and becoming a man, becoming a person. János Székely’s Temptation.
BB: So give us a snapshot of an ordinary moment in your life that gives you real joy, just a Polaroid snapshot.
JK: Waking up, having a cup of coffee, sitting down and working in my notebook, and then easing into an essay, and doing that for a little bit of time. There’s nothing more satisfying than writing some good words. Yeah.
BB: Beautiful. What is one thing you’re deeply grateful for right now?
JK: My family, my husband, yeah.
BB: You’re going to have to help me with some of these songs. We asked you for five songs that you couldn’t live without, and I’m going to read the ones. Okay, I was taken aback by Moby, “Why Does My Heart Feel So Bad?” by Moby from his album Play. “You’ll be Back,” Lin-Manuel Miranda’s Hamilton, the best song. “Let’s Dance” by David Bowie from his album Let’s Dance, and then you said a piano sonata number 32 by Ludwig Beethoven, not because of the song per se, but because the guy was stone deaf when he composed it and therefore performed it, which is incredible, and then tell me about this aria.
JK: The aria yeah, Bellini’s “Norma” is the opera and Act 1 Scene 2, I don’t do Italian but it’s like, [words in Italian] or it’s something about, “Oh and you are the victim.” Anyway, it’s this wonderful aria of a tenor and two sopranos, and the circumstances are, he has betrayed both of them, in other words, one of them is his wife, one of them is his lover, and each finds out, “Oh my God, you’re sleeping with him.” And they all meet and they discover this, and what ensues though, ultimately are the two sopranos, the two women in this aria, where I don’t speak Italian, I don’t know what they’re saying, but you can tell they’ve come together, they’ve… They’ve gone beyond this traitor, and it is one of the most beautiful arias in opera. Yeah, I have “Norma,” the whole opera, but I’ll often go to just that little bit to listen to it.
BB: Okay, so here’s the writer in you. In one sentence, what does this mini mix tape say about you, Jason?
JK: It’s the arc of my life. Once upon a time, I used to have coffee, with cream and sugar. How could you never have it? Now I drink coffee that’s black. The point is, I still drink coffee, but over time you change. I could no sooner drink coffee now with cream and sugar and yet I still drink coffee. What am I getting at? So I agree it’s an eclectic mix, but it reflects… There’s something called Jason there throughout all of that, but over this time, Jason has changed. Yeah, so there’s something that’s Jason in all of those songs, but I will freely admit that the person who is Jason has changed. “Let’s Dance,” I listened to when I was young and really enjoyed it. I still do though, I still do, and this opera I found out a couple of years ago, and I know I hated opera when I was young, I could no sooner listen to opera, but now I do. So I guess I’m a person that’s always open to change and knowing that who I will be later will be different than now, whether or not I get Alzheimer’s. [laughter]
BB: That is beautiful. Thank you so much.
JK: Well, thanks for having me. It was a lot of fun.
BB: Thank you for the work that you do every single day. The Problem of Alzheimer’s is incredible. We’ll tell people where they can get it, and I feel so grateful that you’ve just brought yourself and your heart to this work, and you talk to us about it in a really real way, so thank you.
JK: Thank you so much. It was really great to be here. Hi, everyone. [laughter]
BB: I hope y’all took away as much as I did from this conversation. The book is policy, it’s medicine, it’s stories, and I do think for me, I wish I would have had this when I first started. I was so young trying to help caregive for my grandmother, I was like, “What kind of jacked up system is this? This cannot be… I just must not understand.” And I think something like this would have been so helpful.
BB: You can find The Problem of Alzheimer’s, How Science, Culture, and Politics Turned a Rare Disease into a Crisis and What We Can Do About It, wherever you buy books. We’ll link to it on our episode page. His website is www.jasonkarlawish, K-A-R-L-A-W-I-S-H dot com, and he is @jasonkarlawish on Twitter. Y’all know that every episode of Unlocking Us and Dare to Lead, actually we have episode pages on brenebrown.com where we have resources, links, downloads, and transcripts, usually about five days, five business days after the podcast goes live.
BB: You can also sign up for the Brené Brown newsletter there, where we talk about what’s coming and recap some podcasts and share big news. Grateful to be here on Spotify, there’s a whole Brené Brown hub on Spotify, with all the episodes, my picks, mini mix tapes, playlists, everything in one spot. We’re going to add, some new playlists are coming soon. I’m saying this out loud, so Laura Mayes, who runs the podcasting for us here at Brené Brown Education and Research Group, is a music phenom, fanatic, obsessive person, who makes these incredible monthly playlists and I’m going to start posting them for y’all to enjoy as well.
BB: Now that I’ve said it on the podcast, it must become true. Thanks for being here, y’all. Stay awkward, brave, and kind, and when you’re thinking about healthcare, remember, we’ve got to take care of each other, we are literally all in this together. See y’all next week right here on Spotify.
BB: Unlocking Us is a Spotify original from Parcast. It’s hosted by me, Brené Brown. It’s produced by Max Cutler, Kristen Acevedo, Carleigh Madden, and by Weird Lucy Productions. Sound design by Kristen Acevedo and Andy Waits, and music is by the amazing Carrie Rodriguez, and the amazing Gina Chavez.
© 2021 Brené Brown Education and Research Group, LLC. All rights reserved.